Tachypnea is a common clinical sign in patients with pneumonia, characterized by an abnormally rapid breathing rate. In pneumonia, the infection causes inflammation and fluid accumulation in the lung tissues, leading to impaired gas exchange and decreased oxygen levels. As a result, the respiratory system responds by increasing the breathing rate, often exceeding 20 breaths per minute in adults, to compensate for the reduced oxygenation. Clinicians use tachypnea as a key diagnostic indicator when assessing pneumonia severity and progression. Data shows that respiratory rates above 30 breaths per minute are associated with more severe pneumonia and a higher risk of complications. Monitoring respiratory rate alongside other clinical signs such as fever, cough, and chest pain helps guide treatment decisions and improves patient outcomes.
Table of Comparison
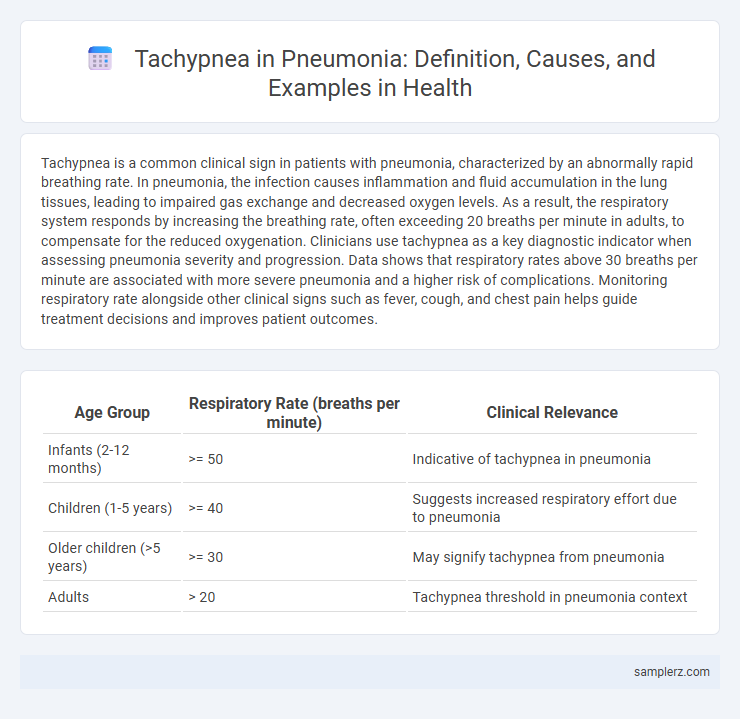
| Age Group | Respiratory Rate (breaths per minute) | Clinical Relevance |
|---|---|---|
| Infants (2-12 months) | >= 50 | Indicative of tachypnea in pneumonia |
| Children (1-5 years) | >= 40 | Suggests increased respiratory effort due to pneumonia |
| Older children (>5 years) | >= 30 | May signify tachypnea from pneumonia |
| Adults | > 20 | Tachypnea threshold in pneumonia context |
Introduction to Tachypnea in Pneumonia
Tachypnea in pneumonia manifests as an abnormally rapid respiratory rate exceeding 20 breaths per minute, signaling compromised lung function due to infection and inflammation. This accelerated breathing serves as a critical clinical marker indicating hypoxemia and increased respiratory effort in patients. Early recognition of tachypnea is vital for prompt diagnosis and effective management of pneumonia-related respiratory distress.
Clinical Definition of Tachypnea
Tachypnea, clinically defined as an abnormally rapid respiratory rate exceeding 20 breaths per minute in adults, is a common symptom observed in pneumonia cases. It reflects the body's response to impaired gas exchange and hypoxia caused by lung inflammation and consolidation. Rapid breathing in pneumonia serves as a critical clinical indicator for severity assessment and guides urgent respiratory support interventions.
Pathophysiology of Tachypnea in Pneumonia
Tachypnea in pneumonia results from impaired gas exchange due to alveolar inflammation and fluid accumulation, leading to hypoxemia that stimulates peripheral chemoreceptors. This triggers an increased respiratory rate as the body attempts to enhance oxygen intake and carbon dioxide elimination. The inflammatory cytokines released during infection further disrupt pulmonary function, exacerbating the rapid breathing response.
Recognizing Tachypnea as a Symptom
Tachypnea, characterized by an abnormally rapid respiratory rate exceeding 20 breaths per minute in adults, commonly presents as a key symptom in pneumonia. Clinicians recognize tachypnea as a critical indicator of respiratory distress due to lung infection, often accompanied by fever, cough, and chest pain. Early identification of tachypnea in pneumonia patients aids prompt diagnosis and intervention, reducing the risk of complications such as hypoxia or respiratory failure.
Case Example: Pediatric Tachypnea in Pneumonia
Pediatric tachypnea in pneumonia commonly presents as rapid breathing exceeding 60 breaths per minute in infants under two months or over 50 breaths per minute in children aged two to twelve months, signaling severity of respiratory distress. This elevated respiratory rate often accompanies other clinical signs such as nasal flaring, chest retractions, and hypoxemia, which necessitate prompt medical intervention to prevent complications. Early recognition of tachypnea in pediatric pneumonia cases improves diagnosis accuracy and guides timely treatment to reduce morbidity and mortality in this vulnerable population.
Case Example: Elderly Patient Tachypnea in Pneumonia
An elderly patient with pneumonia often exhibits tachypnea, characterized by a respiratory rate exceeding 20 breaths per minute, reflecting the body's response to impaired gas exchange and hypoxia. In clinical settings, tachypnea serves as a critical indicator of respiratory distress and the severity of pneumonia, necessitating prompt assessment and intervention. Monitoring respiratory rate alongside oxygen saturation levels enhances the diagnosis and management of pneumonia-induced tachypnea in geriatric patients.
Diagnostic Indicators: Tachypnea Patterns in Pneumonia
Tachypnea in pneumonia typically presents as a respiratory rate exceeding 20 breaths per minute in adults and over 50 in infants, serving as a primary diagnostic indicator. The pattern often correlates with hypoxemia, where increased respiratory effort reflects impaired gas exchange due to alveolar inflammation and consolidation. Monitoring tachypnea alongside oxygen saturation and auscultatory findings improves early pneumonia detection and guides the urgency of clinical intervention.
Risk Factors for Tachypnea in Pneumonia Cases
Tachypnea in pneumonia often arises due to hypoxia and increased respiratory drive caused by alveolar inflammation and fluid accumulation. Risk factors include advanced age, chronic obstructive pulmonary disease (COPD), heart failure, immunosuppression, and delayed antibiotic treatment, which exacerbate respiratory distress. Early recognition of these factors is critical for timely intervention and improved patient outcomes.
Management Strategies for Tachypnea in Pneumonia
Management strategies for tachypnea in pneumonia include supplemental oxygen therapy to maintain adequate oxygen saturation levels above 92%, and the use of bronchodilators to relieve airway obstruction when indicated. Close monitoring of respiratory rate and effort, alongside antibiotic treatment targeted at the pneumonia-causing pathogen, supports resolution of respiratory distress. In severe cases, non-invasive ventilation or mechanical ventilation may be required to ensure proper ventilation and oxygenation.
Prognostic Implications of Tachypnea in Pneumonia
Tachypnea in pneumonia serves as a critical prognostic indicator, frequently correlating with increased disease severity and higher risk of respiratory failure. Elevated respiratory rates above 30 breaths per minute often signal poor oxygenation and systemic distress, necessitating prompt clinical intervention. Monitoring tachypnea helps guide treatment decisions and predict potential complications, improving patient outcomes in pneumonia cases.
example of tachypnea in pneumonia Infographic
 samplerz.com
samplerz.com