Hypertrichosis, characterized by excessive hair growth, can be observed in endocrinology as a result of hormonal imbalances. One common example is congenital adrenal hyperplasia, where abnormal adrenal gland function leads to increased androgen production causing excessive body hair. This condition is often diagnosed through blood tests measuring hormone levels such as 17-hydroxyprogesterone. Another endocrinological cause of hypertrichosis is polycystic ovary syndrome (PCOS), where elevated androgens trigger unwanted hair growth in females. The presence of hypertrichosis in PCOS patients is typically accompanied by other symptoms like irregular menstruation and insulin resistance. Understanding the link between hypertrichosis and endocrine disorders aids in accurate diagnosis and targeted treatment strategies.
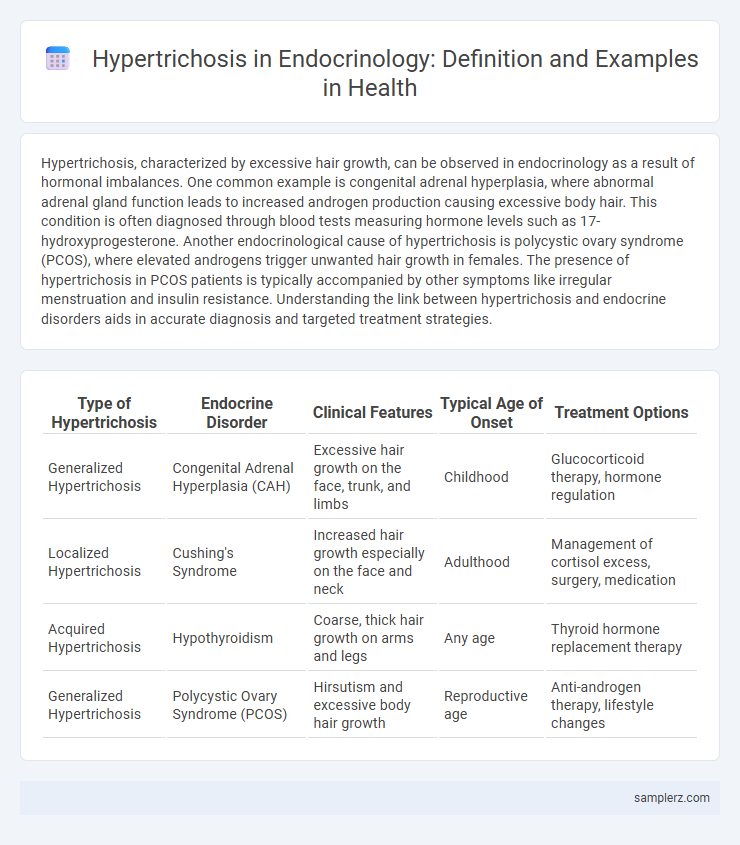
Table of Comparison
| Type of Hypertrichosis | Endocrine Disorder | Clinical Features | Typical Age of Onset | Treatment Options |
|---|---|---|---|---|
| Generalized Hypertrichosis | Congenital Adrenal Hyperplasia (CAH) | Excessive hair growth on the face, trunk, and limbs | Childhood | Glucocorticoid therapy, hormone regulation |
| Localized Hypertrichosis | Cushing's Syndrome | Increased hair growth especially on the face and neck | Adulthood | Management of cortisol excess, surgery, medication |
| Acquired Hypertrichosis | Hypothyroidism | Coarse, thick hair growth on arms and legs | Any age | Thyroid hormone replacement therapy |
| Generalized Hypertrichosis | Polycystic Ovary Syndrome (PCOS) | Hirsutism and excessive body hair growth | Reproductive age | Anti-androgen therapy, lifestyle changes |
Overview of Hypertrichosis in Endocrinology
Hypertrichosis in endocrinology often presents as excessive hair growth due to hormonal imbalances, including conditions like polycystic ovary syndrome (PCOS) and Cushing's syndrome. Androgen excess leads to localized or generalized hypertrichosis, significantly impacting patient quality of life and requiring detailed hormonal evaluation for accurate diagnosis. Effective management involves addressing underlying endocrine disorders and may include pharmacological treatments such as anti-androgens or corticosteroid modulation.
Androgen Excess and Hypertrichosis
Androgen excess frequently leads to hypertrichosis, characterized by excessive hair growth in androgen-sensitive areas such as the face, chest, and back. Conditions like polycystic ovary syndrome (PCOS) and congenital adrenal hyperplasia often involve elevated androgen levels causing this symptom. Managing androgen imbalance through hormonal therapy can significantly reduce hypertrichosis severity in affected patients.
Hypertrichosis in Cushing’s Syndrome
Hypertrichosis in Cushing's Syndrome manifests as excessive, diffuse hair growth due to prolonged exposure to high cortisol levels disrupting normal hair follicle cycling. This endocrine disorder leads to androgen excess and adrenal hyperplasia, which stimulate abnormal hair proliferation on the face, trunk, and extremities. Clinical identification of hypertrichosis in patients with Cushing's Syndrome aids diagnosis and highlights the importance of hormonal balance in hair growth regulation.
Hypertrichosis Associated with Acromegaly
Hypertrichosis associated with acromegaly manifests as excessive hair growth due to prolonged exposure to elevated growth hormone levels originating from pituitary adenomas. This endocrinological disorder leads to thickened, coarse hair predominantly on the face, extremities, and trunk, complicating diagnosis with other hypertrichotic conditions. Early detection through serum insulin-like growth factor-1 (IGF-1) measurement and pituitary imaging is critical for managing hypertrichosis in acromegaly and preventing systemic complications.
Thyroid Disorders and Hypertrichosis Manifestations
Hypertrichosis associated with thyroid disorders often presents as excessive, abnormal hair growth due to imbalances in thyroid hormone levels affecting hair follicle cycle regulation. In hypothyroidism, patients may exhibit coarse, brittle hair and increased vellus hair growth, while hyperthyroidism can lead to fine, soft hypertrichosis predominantly on the face and extremities. These manifestations highlight the critical role of thyroid function in modulating hair follicle activity and the need for careful endocrine evaluation in unexplained cases of hypertrichosis.
Hypertrichosis in Congenital Adrenal Hyperplasia
Hypertrichosis in Congenital Adrenal Hyperplasia (CAH) manifests as excessive, abnormal hair growth due to adrenal gland enzyme deficiencies affecting steroid hormone production. Elevated androgen levels in CAH stimulate hair follicles, resulting in excessive terminal hair on the face, limbs, and trunk, which significantly impacts patients' quality of life. Recognizing hypertrichosis in CAH patients aids endocrinologists in diagnosis, allowing targeted treatments such as glucocorticoid therapy to reduce androgen excess and mitigate hair growth.
Drug-Induced Hypertrichosis in Endocrine Practice
Drug-induced hypertrichosis commonly occurs in endocrine practice due to medications such as minoxidil, phenytoin, and cyclosporine, which stimulate excessive hair growth beyond normal patterns. This condition is frequently observed in patients undergoing treatment for hypertension, epilepsy, or organ transplantation, highlighting the importance of monitoring hair changes during pharmacotherapy. Understanding the pathophysiology of drug-induced hypertrichosis facilitates accurate diagnosis and management in endocrine-related clinical settings.
Differential Diagnosis: Hypertrichosis vs. Hirsutism
Hypertrichosis involves excessive hair growth over the entire body regardless of androgen influence, distinguishing it from hirsutism, which is characterized by androgen-dependent hair growth in a male pattern distribution, mainly in women. Key conditions associated with hypertrichosis include rare congenital syndromes like Ambras syndrome and medication-induced cases such as phenytoin or minoxidil use. Endocrinologists differentiate these disorders by assessing serum androgen levels, clinical hair growth patterns, and potential underlying endocrine abnormalities such as polycystic ovary syndrome (PCOS) in hirsutism versus non-androgenic causes in hypertrichosis.
Clinical Case Examples of Endocrine-Related Hypertrichosis
Clinical case examples of endocrine-related hypertrichosis include polycystic ovary syndrome (PCOS), where excessive androgen production leads to abnormal hair growth patterns on the face, chest, and back. Congenital adrenal hyperplasia (CAH) presents with hypertrichosis due to increased adrenal androgen secretion, often accompanied by ambiguous genitalia in newborns. Another example is Cushing's syndrome, characterized by elevated cortisol levels that can cause coarse, excessive hair growth along with other metabolic disturbances.
Management Strategies for Endocrine Hypertrichosis
Management strategies for endocrine hypertrichosis prioritize identifying and treating underlying hormonal imbalances such as polycystic ovary syndrome (PCOS) or adrenal hyperplasia. Therapeutic approaches include the use of anti-androgens like spironolactone, hormonal contraceptives to regulate androgen levels, and lifestyle modifications targeting weight reduction to improve endocrine function. Laser hair removal and topical eflornithine provide adjunctive cosmetic relief by reducing excessive hair growth.
example of hypertrichosis in endocrinology Infographic
 samplerz.com
samplerz.com